Decoding Diverticulitis: Causes, Symptoms, and Management Strategies
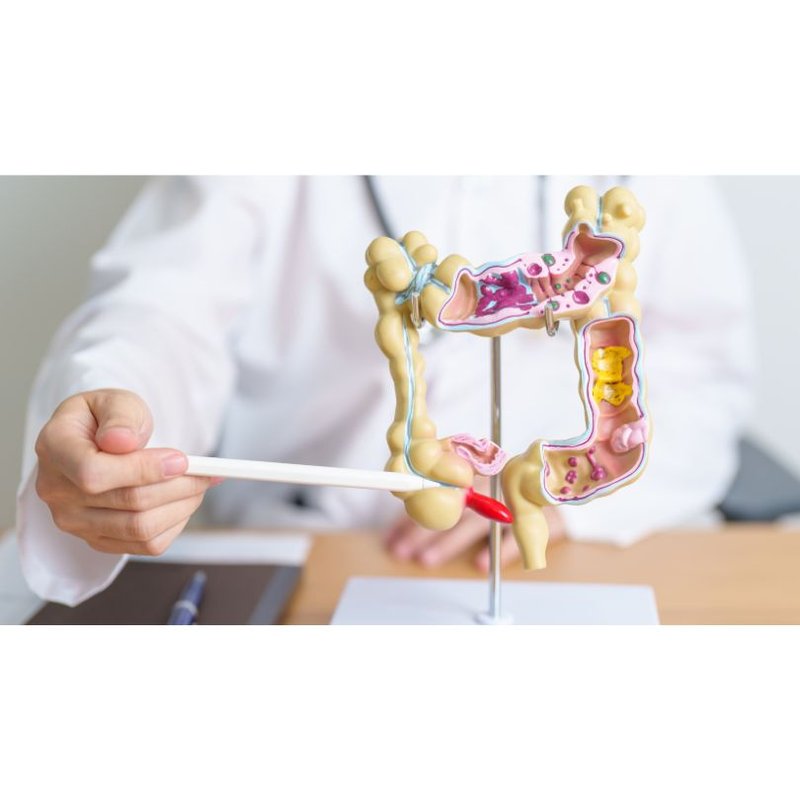
Let’s delve into the intricate realm of diverticular disease as we explore diverticulosis and diverticulitis. Having diverticular disease without any symptoms is known as diverticulosis. However, if these pouches become inflamed or infected, it is called diverticulitis. The main risk factors for diverticular disease include increasing age and eating a western diet low in dietary fibre. This comprehensive exploration sheds light on these conditions affecting the large intestine, offering insights beyond conventional sources to equip you with a comprehensive understanding.
What can trigger diverticulitis?
Your colon is a muscular tube that pushes waste matter down towards your rectum, to be expelled via your anus as stools. The colon uses rhythmic muscular contractions (peristalsis) to propel waste matter along, using its tough outer layer of muscle in a squeezing/pushing movement. The inner layer of your colon is lined with smoother, weaker tissue.
If you eat a diet that is rich in fibre, your stools are large and soft and easily pushed out of your body. If your diet is mainly processed foods that are low in dietary fibre, this can give you constipation, resulting in small, hard stools. These are difficult for your colon to move, needing extra effort and straining on your behalf.
Diverticulitis occurs when small pouches (diverticula) that form in the colon become inflamed or infected. Several factors can trigger diverticulitis, including:
- Obstruction: When waste or stool becomes trapped in the diverticula, it can lead to inflammation and infection.
- Microperforation: Microscopic perforations in the diverticula can allow bacteria from the colon to enter the pouches, triggering an inflammatory response.
- Dietary Factors: A diet low in fibre and high in refined carbohydrates may contribute to diverticulitis by promoting constipation and straining during bowel movements. Foods such as red meat, processed foods, and sugary snacks may exacerbate inflammation.
- Genetics: Some individuals may have a genetic predisposition to developing diverticulitis. Family history and genetic factors can influence the likelihood of developing the condition.
Understanding these triggers can help individuals make informed lifestyle modifications to reduce the risk of diverticulitis episodes.
Risk factors for diverticulitis include:
- Having diverticular disease and a history of constipation;
- Being over 50 years of age and eating mostly foods that are processed and low in fibre;
- Living in a western nation, especially Australia, Europe or North America;
- Being obese and physically inactive;
- Being a smoker, and;
- Using non-steroidal anti-inflammatory pain-relief medications (NSAIDs) such as ibuprofen.
What are the warning signs of diverticulitis?
Recognising the warning signs of diverticulitis is crucial for prompt diagnosis and treatment. Common symptoms include:
- Abdominal Pain: Persistent abdominal pain, often located in the lower left side of the abdomen, is a hallmark symptom of diverticulitis. The pain may be constant or intermittent and can range from mild to severe. It may worsen during bowel movements or when pressure is applied to the abdomen.
- Fever: Fever is a common accompanying symptom of diverticulitis, indicating an inflammatory response or infection. A high fever may suggest a more severe infection or complication.
- Changes in Bowel Habits: Individuals with diverticulitis may experience changes in bowel habits, such as diarrhoea or constipation. Some may also notice an increase in gas or bloating.
- Nausea and Vomiting: Some individuals with diverticulitis may experience nausea and vomiting, particularly if the condition is severe. This may occur due to inflammation and irritation of the gastrointestinal tract.
Seeking medical attention promptly if you experience these symptoms is essential for proper diagnosis and treatment of diverticulitis.
Diagnosing diverticulitis
Diverticular disease often goes undiagnosed and you may only discover you have the condition if you have an acute episode of diverticulitis. In fact, the presence of diverticula is often only discovered during investigative procedures for another bowel condition.
Medical history: Your doctor may ask about your complete health history, including your diet and exercise status.
Physical examination: Your doctor will press the outside of your abdomen to find areas of pain.
Blood tests: A full blood count can be used to screen for infection by measuring your white blood cell count. Other blood tests may include liver, pancreatic and kidney function tests, as well as inflammation markers. If other conditions are suspected, blood tests may be ordered to help exclude these.
Stool culture: A stool microscopy, culture and sensitivity is used to check if there are harmful bacteria in your faeces. You will be given a sterile container to provide a fresh stool sample. In the lab, a scientist will look for bacteria under a microscope and place some of your stool onto a special gel (agar) plate, which will selectively grow certain bacteria. The stool may also be tested for the presence of blood.
CT Scan: CT scans send X-ray beams from multiple angles using a machine that circles your body. This allows the machine to generate cross-sectional images of your internal organs. Often a contrast dye will be injected into your veins before the scan, and/or ingested or given as an enema if the scan is of the abdominal area, to help get a clearer picture of the digestive system. Abdominal scans also require fasting for 2-4 hours prior. The whole procedure takes about 30 minutes. A CT scan can help diagnose diverticulitis and its potential complications.

Barium enema: A barium enema is a diagnostic procedure that uses a contrasting barium dye and X-ray to examine your bowels. Before the procedure, the bowel will be prepared by being flushed out with an oral laxative solution and/or enema. A barium-filled tube is then inserted into the anus and the fluid released into the colon. Air will be pumped in to ensure the fluid reaches the corners of the bowel. An X-ray is then taken of the inflated bowel and it may show if diverticula are present.
Colonoscopy: A colonoscopy is used to examine the entire length of your colon. On the day before your procedure your doctor will prescribe a suitable oral laxative solution to clear your bowel of faeces, to allow the clearest view of the bowel. You will generally need to drink a lot of water during the preparation as you will pass large amounts of loose and sometimes watery stools. During the colonoscopy, a long, thin tube with a camera, called a colonoscope, is inserted into your bowel through your anus. You will be sedated prior to the procedure to help you to relax.
Types of treatment
Your doctor will be able to advise if treatment at home is suitable. Sometimes diverticulitis is a medical emergency that requires immediate hospitalisation for assessment and management.
Home care: Home care usually incorporates the following:
Liquid diet: You may be advised to have a liquid-only diet for a few days, to allow your bowel to rest and give it time to recover.
Pain-relief medications: You will most likely be given paracetamol or other pain-relief medication to help with your pain. Non-steroidal anti-inflammatories (NSAIDs) such as ibuprofen and aspirin are not recommended, as they can increase your chance of internal bleeding and upset your stomach.
Antibiotics: Antibiotics are likely to be prescribed to fight the infection in your bowel.
Hospital treatment: Hospital treatment may be necessary if you have an acute and severe case of diverticulitis with the following circumstances:
- Your pain is too extreme to be treated with simple pain-relief medications at home;
- You cannot take antibiotics in tablet form, or they are not effective;
- You are severely dehydrated or in poor health;
- You have not seen any improvement after two days of home treatment;
- You have a weakened immune system that puts you at risk of infections, and;
- Your care team is concerned you may develop complications.
Intravenous liquids and medications: Treatment is likely to include fluids and antibiotics, given via an intravenous drip (IV) attached to a vein in your arm. Pain-relief medications can also be given intravenously or via muscular injection. Recovery usually occurs over a few days, but can depend on the severity of your condition.
Surgery: Surgery is usually only required in certain cases of diverticulitis. If there are certain complications, frequent episodes of infection and/or a severe infection not responding to medications, surgery may be indicated. Surgical treatment can comprise the following:
Bowel resection: Bowel resection is a type of surgery in which the affected part of your bowel is removed. You will be under general anaesthetic during the surgery, so will not feel any pain. Once the unhealthy part of your bowel is removed, your surgeon will either staple or sew the healthy parts together. You will probably be kept in hospital for 3-7 days after surgery and receive fluids via an IV drip for the first few days. Food is generally gradually reintroduced as tolerated.
Stoma surgery: Your surgeon may decide to give your bowel time to heal before reattaching it, either temporarily or permanently (rarely). This can be done by creating a special opening, called a stoma, in your abdomen. Your faecal matter passes through this opening into a special bag. You will usually undergo surgery to reattach your bowel once the bowel has healed.
Potential complications
There are a number of potentially serious complications of diverticulitis:
Perforation - this is when your bowel wall ruptures, allowing its contents to escape into your abdominal cavity. This is a life-threatening situation requiring immediate surgery;
Abscess - this is a collection of pus that forms in an area where you have developed an infection. If the abscess bursts, it can cause blood infection (sepsis) or bowel perforation;
Fistula - an abnormal channel that forms between two areas of the body not supposed to be connected, such as your bowel and bladder;
Peritonitis - infection of the lining of your abdominal cavity requiring immediate treatment. It often happens if an abscess bursts or if a bowel perforation occurs;
Intestinal obstruction - a blockage of your bowel, stopping the passage of both liquids and solids;
Sepsis (septicaemia) - this happens when an infection spreads throughout your bloodstream, and;
Haemorrhage - uncontrolled bleeding, usually due to a blood vessel rupturing near your diverticula. Surgery may be required to stem the bleeding.
What is the life expectancy with diverticulitis?
The life expectancy of individuals with diverticulitis largely depends on various factors, including the severity of the condition, overall health, and response to treatment. In most cases, diverticulitis is a manageable condition, and with proper medical management and lifestyle modifications, individuals can lead fulfilling lives.
Complications of diverticulitis, such as abscess formation, perforation, or fistula formation, can impact life expectancy and may require surgical intervention. However, with timely medical care and appropriate treatment, the prognosis for individuals with diverticulitis is generally favourable.

What foods should you avoid if you have diverticulitis?
Dietary modifications play a crucial role in managing diverticulitis and preventing flare-ups. While dietary recommendations may vary for each individual, some general guidelines include:
- High-Fibre Foods: A diet rich in fibre can help promote regular bowel movements and prevent constipation, reducing the risk of diverticulitis flare-ups. High-fibre foods include fruits, vegetables, whole grains, and legumes.
- Low-FODMAP Foods: Some individuals with diverticulitis may benefit from following a low-FODMAP diet to reduce symptoms such as bloating and gas. Low-FODMAP foods include certain fruits, vegetables, grains, and dairy products.
- Hydration: Adequate hydration is essential for maintaining bowel regularity and preventing constipation. Drinking plenty of water throughout the day can help soften stools and ease bowel movements.
- Limiting Certain Foods: While there is no strict "diverticulitis diet," individuals may benefit from avoiding certain foods that can exacerbate symptoms or trigger flare-ups. These may include spicy foods, nuts, seeds, popcorn, and high-fat foods.
Consulting with a healthcare professional or registered dietitian can help individuals develop a personalised dietary plan tailored to their specific needs and preferences.
Have you got more questions about your health? With Health&'s user-friendly personal health assistant, you can easily navigate through a series of simple questions to receive tailored support in just minutes.
Health& makes it easy to simply enter your search query in our A-Z library of medically-verified health content, ensuring you find the best matches for your situation. Explore more health content, take early-intervention risk assessments, store your medical records and more! Discover the support you need with the Health& app, empowering you on your journey towards living better, longer.

