Scoliosis is the sideways curve of the spine. It is a common condition, affecting about 2-3% of the population to some degree. Early intervention can help lessen the severity of scoliosis, using physiotherapy, good posture practice and possibly a brace.…
Ankylosing spondylitis
What is ankylosing spondylitis?
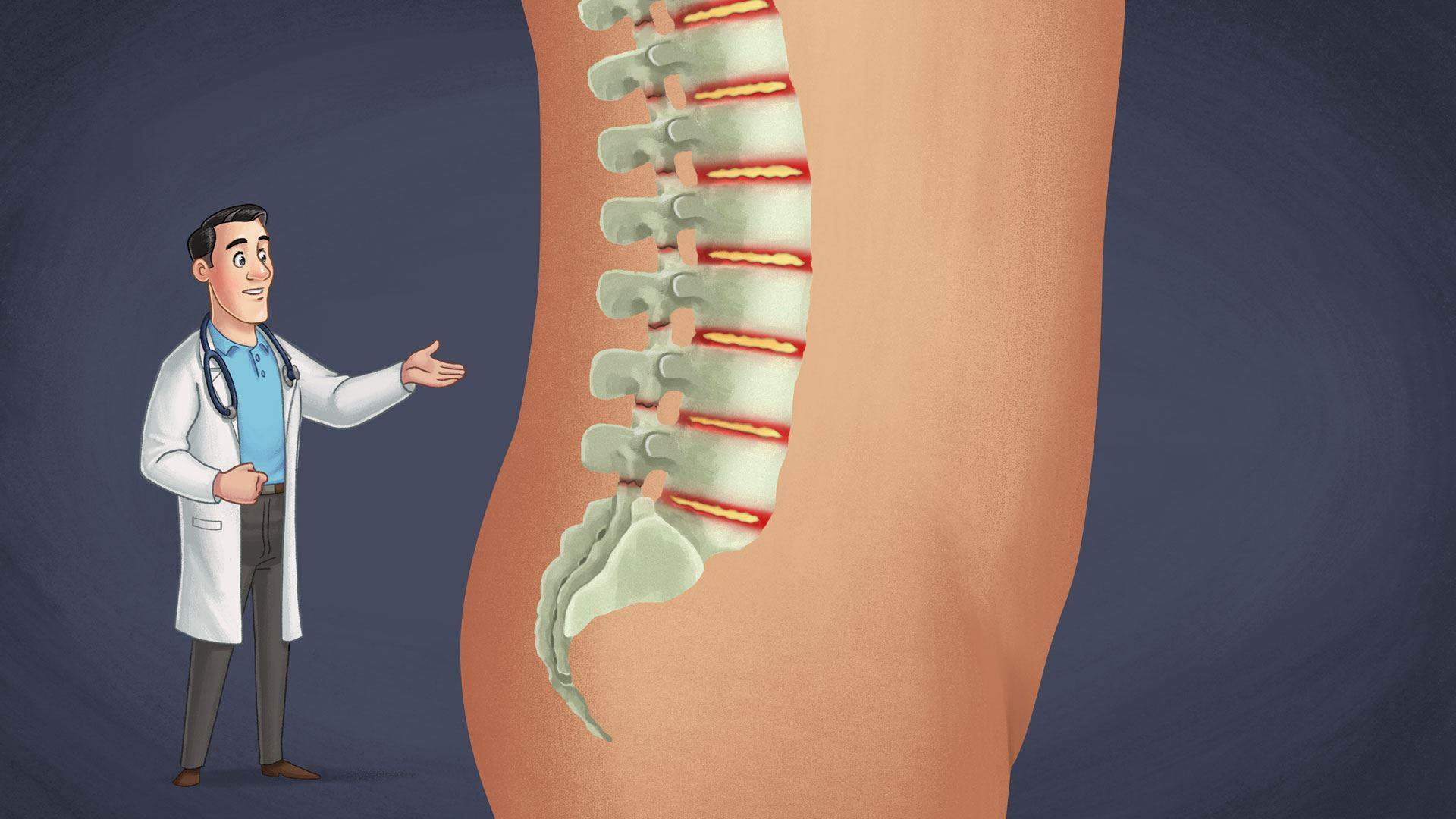
Ankylosing spondylitis is a form of inflammatory arthritis. It affects the joints of the spine, in particular the sacroiliac joint at the bottom of the spine. Ankylosing spondylitis causes the swelling of the ligaments, discs and joints between the vertebrae of the spine. Symptoms include pain and stiffness in the lower back and over time, fusion of the vertebrae can occur.
Discs
Intervertebral discs - layers of cartilaginous material that act as cushions between the vertebrae and the joints in the spine, enabling the spine to bend and twist.
Sacroiliac joint
The joint that connects the spine to the pelvis.
Vertebrae
The bones that make up the spinal column.
Inflammatory arthritis
A group of conditions in which the body's immune system mistakenly attacks the joints. It can also affect other tissues and organs.
Causes
The specific cause of ankylosing spondylitis is unknown, although genetic factors appear to play a role. The presence of a specific gene that produces the antigen HLA-B27, is found in nine out of 10 people with ankylosing spondylitis, although there are people with the gene that do not develop the condition. It is therefore thought that other factors are involved in triggering ankylosing spondylitis.
Ankylosing spondylitis can begin to develop from the age of 15 years and generally affects young adults before the age of 35 years. The condition begins with inflammation of the sacroiliac joint and facet joint. Over time, bony growths can begin to form and cause fusion of vertebrae, causing limited movement and pain in the lower back.
 Ankylosing spondylitis causes the swelling of the ligaments, discs and joints between the vertebrae of the spine.
Ankylosing spondylitis causes the swelling of the ligaments, discs and joints between the vertebrae of the spine. Discs
Intervertebral discs - layers of cartilaginous material that act as cushions between the vertebrae and the joints in the spine, enabling the spine to bend and twist.
Facet joint
Small joints that are located between and behind each vertebrae in the spine.
HLA-B27
A type of antigen associated with particular inflammatory diseases.
Inflammation
A body’s protective immune response to injury or infection. The accumulation of fluid, cells and proteins at the site of an infection or physical injury, resulting in swelling, heat, redness, pain and loss of function.
Sacroiliac joint
The joint that connects the spine to the pelvis.
Vertebrae
The bones that make up the spinal column.
Golder, V. (2013) Ankylosing spondylitis: an update. Australian Family Physician 42:780-784. Accessed 16 October 16 2014, from
External linkRisk factors
Risk factors associated with developing the condition include:
- Having the HLA-B27-causing gene increases the susceptibility of developing ankylosing spondylitis;
- Family history of the condition increases the risk of passing on the HLA-B27-causing gene, and;
- Being male - it is three times more common in men than women.
HLA-B27
A type of antigen associated with particular inflammatory diseases.
Golder, V. (2013) Ankylosing spondylitis: an update. Australian Family Physician 42:780-784. Accessed 16 October 16 2014, from
External linkSigns and symptoms
The signs and symptoms of ankylosing spondylitis include:
- Lower back pain that gradually appears over time, is worse after rest and improves after exercise;
- Stiffness that worsens in the morning;
- Buttock, hip or shoulder pain;
- Limited mobility of the spine;
- Head-forward posture or neck pain;
- Pain in ligaments and tendons that are attached to the spine, for example, the back of the heel, and;
- Eye pain, light sensitivity or blurred vision.
The signs and symptoms can improve, worsen, or stop entirely at irregular intervals.
Golder, V. (2013) Ankylosing spondylitis: an update. Australian Family Physician 42:780-784. Accessed 16 October 16 2014, from
External linkMethods for diagnosis
Identifying ankylosing spondylitis early is important in preventing any damage to the spine. In many cases there can be a delay of 5-7 years from the time symptoms first appear to when the condition is diagnosed. In addition to reviewing the medical history, diagnosis of ankylosing spondylitis can be determined by the following tests:
- A physical examination;
- An X-ray to identify any changes in bones and joints;
- A computerized tomography (CT) scan to assist with early diagnosis;
- A magnetic resonance imaging (MRI) scan to enable visualization of the inflammatory changes in the spine;
- Blood tests to check for evidence of inflammation, and;
- Genetic testing to check for the presence of the HLA-B27-causing gene.
Blood tests
During a blood test, blood can be drawn using a needle or by a finger prick. Your blood can then be analyzed to help diagnose and monitor a wide range of health conditions.
Computerized tomography
A scan that uses X-rays to create a 3D image of the body. This can detect abnormalities more effectively than a simple X-ray can.
HLA-B27
A type of antigen associated with particular inflammatory diseases.
Inflammation
A body’s protective immune response to injury or infection. The accumulation of fluid, cells and proteins at the site of an infection or physical injury, resulting in swelling, heat, redness, pain and loss of function.
MRI
A type of imaging that uses a magnetic field and low-energy radio waves, instead of X-rays, to obtain images of organs.
X-ray
A scan that uses ionizing radiation beams to create an image of the body’s internal structures.
Golder, V. (2013) Ankylosing spondylitis: an update. Australian Family Physician 42:780-784. Accessed 16 October 16 2014, from
External linkTypes of treatment
Currently there is no cure for ankylosing spondylitis. The main goal of treatment is to maintain a good quality of life by managing the symptoms and reducing the progression of the condition. Treatments include medications, physiotherapy and surgery.
Medications
Medications used in the treatment of ankylosing spondylitis include:
- Non-steroidal anti-inflammatory drugs (NSAIDs) to reduce inflammation and control pain and stiffness;
- Disease-modifying antirheumatic drugs (DMARDs), which can slow the progression of the condition;
- Tumor necrosis factor (TNF) inhibitors to control inflammation, and;
- Corticosteroids.
Physiotherapy
Physiotherapy is also commonly used to manage ankylosing spondylitis. This can include using specific exercises to reduce the pain and increase the strength and flexibility of the muscles and tendons in the affected area. Your doctor or physiotherapist can tailor an exercise program and other therapies, such as hydrotherapy, to help improve mobility of the spine.
Surgery
In most cases, surgery is not necessary, but can be utilized if there is extreme pain or joint damage. Joints can be surgically fused or repaired, depending on the location and degree of damage to a joint.
Antirheumatic
Drugs used to treat inflammatory arthritis.
Corticosteroids
A medication that resembles the cortisol hormone produced in the brain. It is used as an anti-inflammatory medication.
Hydrotherapy
A water-based type of therapy, used for relaxation and physical rehabilitation.
Inflammation
A body’s protective immune response to injury or infection. The accumulation of fluid, cells and proteins at the site of an infection or physical injury, resulting in swelling, heat, redness, pain and loss of function.
Golder, V. (2013) Ankylosing spondylitis: an update. Australian Family Physician 42:780-784. Accessed 16 October 16 2014, from
External linkPotential complications
In severe forms of ankylosing spondylitis, it is possible for sections of the spine to become fused, causing stiffness and immobility. This can cause the natural curves of the spine to straighten, forcing the body into a hunched position. The rib cage can also become stiff, which can reduce the capacity of the lungs and cause breathlessness. Osteoporosis is a common complication, which can increase the risk of sustaining a fracture.
Ankylosing spondylitis can also increase the risk of developing heart disease and uveitis, a condition involving inflammation of the eye.
Heart disease
A class of diseases that involves the dysfunction of the heart and/or the blood vessels.
Fracture
A complete or incomplete break in a bone.
Inflammation
A body’s protective immune response to injury or infection. The accumulation of fluid, cells and proteins at the site of an infection or physical injury, resulting in swelling, heat, redness, pain and loss of function.
Uveitis
Inflammation of the uvea, the middle inner layer of the eye consisting of the iris, ciliary body and choroid.
Golder, V. (2013) Ankylosing spondylitis: an update. Australian Family Physician 42:780-784. Accessed 16 October 16 2014, from
External linkPrognosis
The prognosis can depend on how early the condition is diagnosed. In some cases, only mild symptoms are experienced at irregular intervals and full physical activity is possible. In other cases, symptoms can be more frequent and complications, including spinal fusion, can occur. Treatment with medications and physiotherapy are important, after a confirmed diagnosis, to achieve the best outcome.
Golder, V. (2013) Ankylosing spondylitis: an update. Australian Family Physician 42:780-784. Accessed 16 October 16 2014, from
External linkPrevention
There are no specific ways to prevent ankylosing spondylitis. It is, however, possible to slow its progression and minimize risk of developing complications through early diagnosis and timely use of specific treatments.
Golder, V. (2013) Ankylosing spondylitis: an update. Australian Family Physician 42:780-784. Accessed 16 October 16 2014, from
External link





